Media Center
Falling Arches: Adult Acquired Flatfoot Deformity
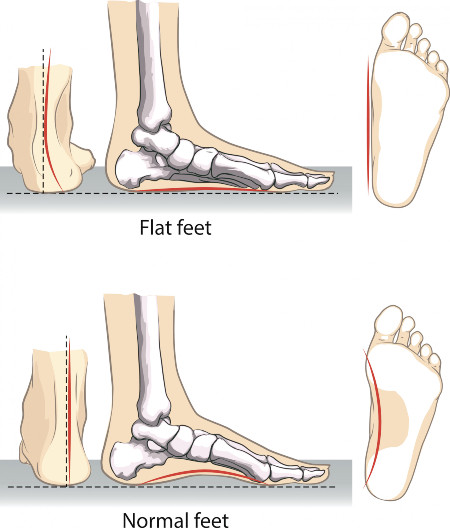
 Despite concerns over the shape of one’s foot, most flat feet do not cause dysfunction and are typically considered within the range of normal, thus not needing treatment. Indeed, many professional athletes have what is defined as a flat foot. All children begin life with flat feet. However, as we mature, the arch of the foot develops. In the adult population, approximately 20-30% of people have flat feet, but most experience no symptoms.
Despite concerns over the shape of one’s foot, most flat feet do not cause dysfunction and are typically considered within the range of normal, thus not needing treatment. Indeed, many professional athletes have what is defined as a flat foot. All children begin life with flat feet. However, as we mature, the arch of the foot develops. In the adult population, approximately 20-30% of people have flat feet, but most experience no symptoms.
Adult acquired flatfoot deformity (AAFD) encompasses a range of disorders leading to progressive loss of the arch of the foot. This is differentiated from the typical flatfoot in that it is painful, and worsens with time. Patients typically complain of a vague pain on the inner part of the ankle joint due to inflammation and degeneration of the posterior tibial tendon. The pain worsens throughout the day and is often relieved with rest. With time, as the arch flattens, the foot begins to roll inward. As the deformity progresses, pain is typically experienced on the outside of the ankle as the heel continues to roll outward.
There are many causes of AAFD. These may include degeneration of the posterior tibial tendon, previous trauma to the foot or ankle, muscle imbalance from neuromuscular disorders, inflammatory disorders such as rheumatoid arthritis, and Charcot arthropathy. AAFD has also been associated with hypertension, obesity, diabetes, and exposure to steroids.
If conservative treatment is unsuccessful, multiple surgical alternatives exist. The surgical procedures fall into one of two categories: 1) joint sparing procedures and 2) fusions. If the joints are still moveable, joint sparing procedures are utilized. This typically involves cutting the calcaneus (i.e., heel bone) and shifting it to realign the heel. Sometimes the calcaneus bone is cut and a block of bone is placed on the outside portion to change the position of the foot. In addition, the dysfunctional posterior tibial tendon is replaced by transferring another tendon to take its place. Often, the achilles tendon is lengthened as well.
If the foot is rigid and not easily correctable, the foot is realigned and the arch restored by fusing joints. In this procedure, screws are placed across the joints to hold them into the appropriate position while the bones grow together. These screws are not usually removed, unless they cause discomfort.
AAFD is a progressive flattening of the arch that causes pain and difficulty walking. When diagnosed early, up to 2/3 of patients can be treated successfully with conservative management. For those who continue to have pain despite appropriate treatment, surgical alternatives exist to restore the arch and function of the foot.