Media Center
What is Hip Impingement?
Introduction
One of my mentors used to always say, “The eyes don’t see what the mind doesn’t know.”
 Hip impingement, also know as femoroacetabular impingement or FAI, in many ways embodies that saying. It has undoubtedly been around for as long as humans, but was only first described as a medical condition in the 1990’s.4 Since being first described, recognition of this common condition has increased exponentially,2 i.e. we are finally “seeing” FAI because we know it exists.
Hip impingement, also know as femoroacetabular impingement or FAI, in many ways embodies that saying. It has undoubtedly been around for as long as humans, but was only first described as a medical condition in the 1990’s.4 Since being first described, recognition of this common condition has increased exponentially,2 i.e. we are finally “seeing” FAI because we know it exists.
Who Is At Risk?
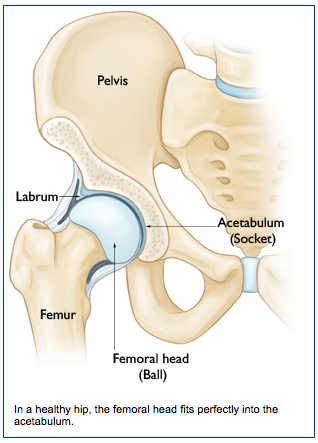
The hip joint is composed of the femoral head (upper end of the femur or thigh bone) and acetabulum (hip socket) (Figure 1). The hip joint is lined by a smooth surface called articular cartilage, which allows movement of the ball in the socket without excessive friction. The acetabulum is surrounded by a ring of tissue known as the labrum that is important for hip stability and holding fluid inside the joint.
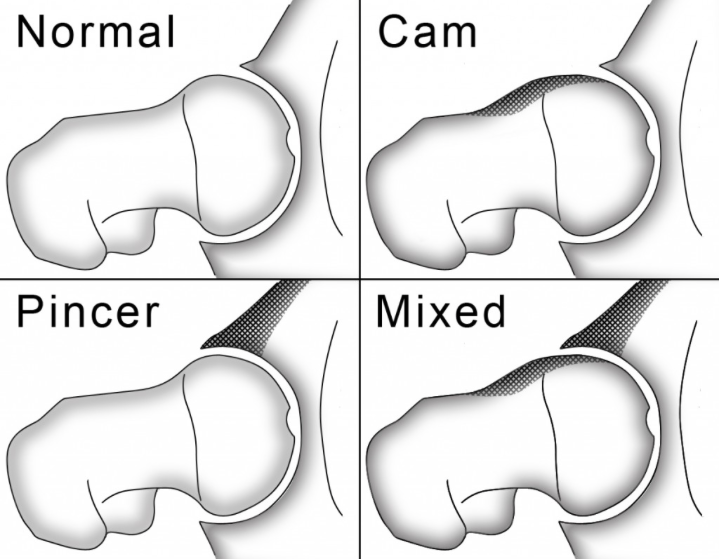
Hip impingement occurs when there is an abnormally shaped femoral head or acetabulum, which causes these bones to rub against each other during range-of-motion of the hip, resulting in joint damage.3 The two most common types of bony abnormalities that cause impingement are “cam” and “pincer” impingement (Figure 2).
- Cam impingement occurs when there is an enlargement of bone on the outside portion of the femoral head, causing it to not be round. As the hip is flexed, this non-round portion of the femoral head produces a shearing force to the articular cartilage. Over time, repetitive shearing with day-to-day activities causes breakdown of the cartilage and labrum, resulting in pain.
- Pincer impingement occurs when the acetabulum is too large and covers too much of the femoral head. As a result of this over coverage, the labrum is pinched by the femur with hip flexion, eventually resulting in labral tearing and articular cartilage damage.
While either type of impingement can occur in an individual, cam impingement is most commonly seen in 20 – 30 year old men, while pincer impingement is more common in women between 30-40 years old.1
Symptoms
The most common presentation of hip impingement is groin pain that occurs with squatting or twisting maneuvers. Patients commonly complain of a dull ache or catching in the hip after activities that involve repetitive hip flexion. Most often, symptoms develop gradually over several weeks or months, but symptoms can also occur acutely with trauma.
Diagnosis
A detailed history and physical exam are essential to the accurate diagnosis of hip impingement. If FAI is suspected based on the history and exam, X rays and an MRI are then performed to determine the type of impingement and associated injuries to the hip, such as damage to the labrum (Figure 3) and/or articular cartilage.
Treatment Options
- Conservative Treatment – Initial treatment of FAI starts with conservative measures, such as activity modification (avoiding painful activities for a period of time), anti-inflammatory medications, physical therapy, and possibly hip injections.
- Surgical Treatment – If a trial of conservative treatment is ineffective at relieving the pain, surgery is an effective treatment for FAI. Surgery is performed arthroscopically (a minimally invasive technique that uses small incisions and a camera to look into the joint) to remove excessive bone that is causing the impingement. After correcting the bony deformity, if the labrum is torn it can be repaired with anchors that secure the tissue back down to the bone.
Into the Future
At TOA we take a personalized approach to both conservative and surgical treatment of hip impingement. We are now using sophisticated computer software (Dyonics Plan, Smith & Nephew (http://www.youtube.com/watch?v=7EJM1j37tEU) to simulate hip motions and determine the exact location of impingement (we will be talking about how this works in a future blog). This powerful tool not only allows us to pin point the location of impingement, it also allows us to determine the amount of bone resection at each area to restore normal anatomy and hip motion. We are also using the latest 3D printing technology (http://www.3dsystems.com/solutions/healthcare) to print life-sized models of patient’s hips as a “hands on” pre-operative assessment and planning tool.
References:
1. Beck M, Kalhor M, Leunig M, Ganz R. Hip morphology influences the pattern of damage to the acetabular cartilage. J Bone Joint Surg Br. 2005;87(7):1012–1018. doi:10.1302/0301-620X.87B7.
2. Botser IB, Smith TW, Nasser R, Domb BG. Open Surgical Dislocation Versus Arthroscopy for Femoroacetabular Impingement: A Comparison of Clinical Outcomes. YJARS. 2011;27(2):270–278. doi:10.1016/j.arthro.2010.11.008.
3. Ganz R, Parvizi J, Beck M, Leunig M, Nötzli H, Siebenrock KA. Femoroacetabular impingement: a cause for osteoarthritis of the hip. Clinical Orthopaedics and Related Research. 2003;(417):112–120. doi:10.1097/01.blo.0000096804.78689.c2.
4. Myers SR, Eijer H, Ganz R. Anterior femoroacetabular impingement after periacetabular osteotomy. Clinical Orthopaedics and Related Research. 1999;(363):93–99.